- Oak Brook:(630) 705-9999
- Chicago:(312) 920-8822
- Email:inquiry@vervecollege.edu
- Make a Payment
- Home
- Programs
- Admission
- Resources
- ATI Entrance Exam Resources
- New E-Digital Library
- Refer a Friend
- School Newsletter
- Events
- Employers
- Job-Network
- Alpha Beta Kappa Candidates
- Verve College Library
- Graduation and Pinning Ceremony Photo Galleries
- Textbook Information
- Career Services
- Tutoring
- School Catalog
- FAQ
- Constitution Day Program
- Alumni
- Verve College Plans
- Financial Aid
- HEERF Reporting
- Satisfactory Academic Progress
- Apply For Financial Aid
- Net Price Calculator
- Return of Title IV Funds (R2T4)
- Financial Aid Office Code of Conduct
- Contact
- FAQs
- Verification Policy
- Vaccination Policy
- Student Right-to-Know Act
- Misrepresentation
- Information Security Program
- Academic Award Year
- Availability of Employee
- Cost of Attendance
- Health & Safety Exemption Requirement
- Students Rights and Responsibilities
- Leave of Absence
- Pell Formula
- Military Students
- Grants/ Scholarship Policy
- Contact Us
- Testimonials
- Blog
Is a Nursing Career Right For You?
Take The Free Quiz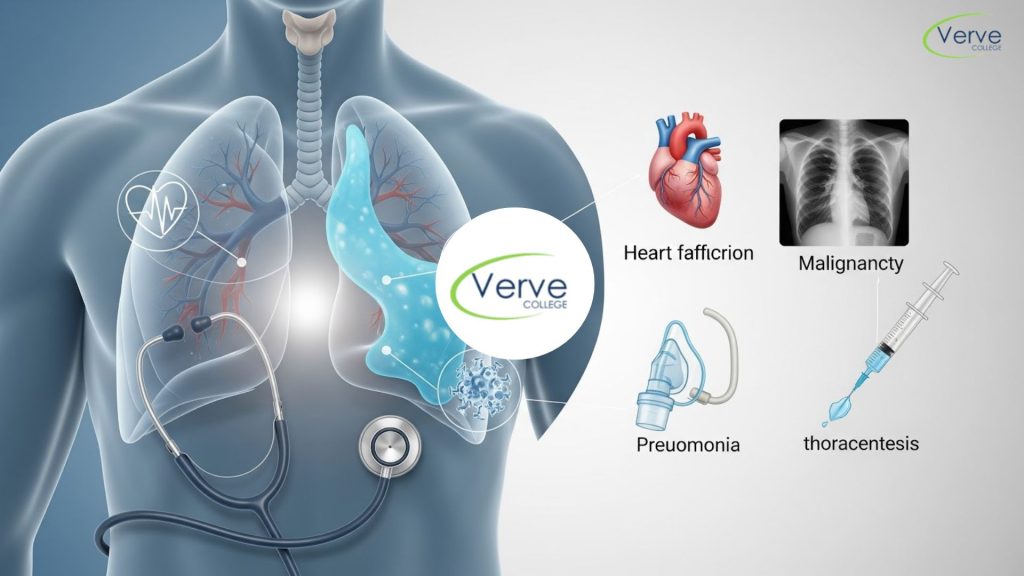
Pleural Effusion: Causes, Symptoms, Diagnosis, and Care
Pleural Effusion: Causes, Symptoms, Diagnosis, and Care
Pleural effusion, commonly described as fluid in lungs pleural effusion, is a condition where excess fluid builds up in the pleural space, the thin gap between the lungs and chest wall. According to global respiratory health data, pleural effusion affects millions of patients every year and is frequently seen in hospital settings, especially among older adults and patients with heart, lung, or kidney conditions.
Understanding this condition is essential for healthcare students and caregivers because pleural effusion is often a sign of an underlying disease, not a disease itself. Learning how and why fluid accumulates helps students connect theory with real clinical situations, especially for those enrolled in anatomy and physiology classes near me, where respiratory mechanics and fluid balance are core topics.
Key Takeaways
- Pleural effusion occurs when excess fluid collects around the lungs, affecting breathing
- Causes range from heart failure to infections and lung diseases
- Symptoms may be mild or severe, depending on fluid amount of fluid
- Diagnosis relies on imaging and fluid analysis
- Care focuses on treating the cause and relieving symptoms
What is Pleural Effusion and How Does It Develop?
Pleural effusion happens when the normal balance of fluid production and absorption in the pleural space is disrupted. Normally, a small amount of fluid helps the lungs move smoothly during breathing. When the body produces too much fluid or cannot absorb it properly, fluid starts to accumulate.
From a physiological standpoint, pleural effusion signifies challenges with circulation, inflammation, or lymphatic drainage concepts being usually closely studied in an A&P nursing class, where candidates learns about connections between various systems in the body during any conditions.
Common Causes of Fluid in the Lungs: Pleural Effusion
The causes of pleural effusion are generally grouped into two categories: transudative and exudative effusions. Transudative effusions are usually caused by systemic conditions such as heart failure or liver disease, where pressure imbalances push fluid into the pleural space.
Exudative effusions result from inflammation or injury. These are commonly linked to pneumonia, tuberculosis, lung cancer, or pulmonary embolism. Infections increase blood vessel permeability, allowing protein-rich fluid to leak into the pleural cavity. Identifying the cause is critical because treatment depends entirely on what is driving the fluid accumulation.
Signs and Symptoms Patients May Experience
Symptoms vary based on how quickly fluid builds up and how much fluid is present. Small effusions may cause no symptoms and are often discovered incidentally on imaging. Larger effusions typically lead to noticeable breathing difficulties.
Common symptoms include shortness of breath, chest pain that worsens with deep breathing, dry cough, and fatigue. In severe cases, patients may struggle to speak in full sentences or feel constant chest pressure. Clinically, symptom assessment helps healthcare providers decide how urgently the fluid needs to be drained and whether immediate intervention is required.
How is Pleural Effusion is Diagnosed?
Diagnosis begins with a physical examination, where reduced breath sounds or dullness on chest percussion may be noted. Imaging plays a central role chest X-rays can detect moderate to large effusions, while ultrasound helps identify smaller fluid collections and guides procedures.
CT scans provide detailed views and help identify underlying lung disease. In many cases, a procedure called thoracentesis is performed to remove fluid for laboratory analysis. Studying the fluid’s color, protein content, and cell count helps determine whether the effusion is caused by infection, cancer, or systemic disease.
Care and Management Approaches
Managing pleural effusion focuses on two goals: relieving symptoms and treating the underlying cause. Mild cases may only require monitoring and medication, such as diuretics for heart-related effusions.
More severe cases require fluid drainage to improve breathing. This may involve thoracentesis or, in recurring cases, longer-term solutions like chest tube placement. Patient care also includes monitoring oxygen levels, managing pain, and educating patients about warning signs. Understanding these care principles is essential for learners preparing through an anatomy and physiology course near me, where applied clinical reasoning is emphasized.
Fluid in Lungs Pleural Effusion: Clinical Importance for Healthcare Learners
From an educational perspective, fluid in the lungs pleural effusion is a key example of how multiple body systems interact during disease. It highlights the connection between cardiovascular health, respiratory mechanics, and fluid regulation.
For nursing and allied health students, this condition strengthens skills in patient assessment, diagnostic interpretation, and care planning. Recognizing pleural effusion early can significantly improve patient outcomes, making it an important topic in foundational healthcare education.
Conclusion
Pleural effusion is more than just excess fluid; it is a clinical sign that points to deeper health issues. Understanding fluid in the lungs, pleural effusion helps healthcare students and caregivers recognize symptoms early, support accurate diagnosis, and deliver effective care. From identifying causes to managing patient comfort, this condition bridges theory and real-world practice. Building strong knowledge in this area prepares learners to respond confidently in clinical settings and reinforces the importance of integrated body system understanding.
FAQs
- Can pleural effusion go away on its own?
Yes, mild pleural effusions may resolve once the underlying condition is treated, such as controlling heart failure or infection. - Is pleural effusion always related to lung disease?
No, it can also be caused by heart, liver, kidney conditions, or systemic inflammation. - Does pleural effusion always require surgery?
No, many cases are managed with medication or simple fluid drainage without surgery.
 Sign up
Sign up Login
Login