- Oak Brook:(630) 705-9999
- Chicago:(312) 920-8822
- Email:inquiry@vervecollege.edu
- Make a Payment
- Home
- Programs
- Admission
- Resources
- ATI Entrance Exam Resources
- New E-Digital Library
- Refer a Friend
- School Newsletter
- Events
- Employers
- Job-Network
- Alpha Beta Kappa Candidates
- Verve College Library
- Graduation and Pinning Ceremony Photo Galleries
- Textbook Information
- Career Services
- Tutoring
- School Catalog
- FAQ
- Constitution Day Program
- Alumni
- Verve College Plans
- Financial Aid
- HEERF Reporting
- Satisfactory Academic Progress
- Apply For Financial Aid
- Net Price Calculator
- Return of Title IV Funds (R2T4)
- Financial Aid Office Code of Conduct
- Contact
- FAQs
- Verification Policy
- Vaccination Policy
- Student Right-to-Know Act
- Misrepresentation
- Information Security Program
- Academic Award Year
- Availability of Employee
- Cost of Attendance
- Health & Safety Exemption Requirement
- Students Rights and Responsibilities
- Leave of Absence
- Pell Formula
- Military Students
- Grants/ Scholarship Policy
- Contact Us
- Testimonials
- Blog
Is a Nursing Career Right For You?
Take The Free Quiz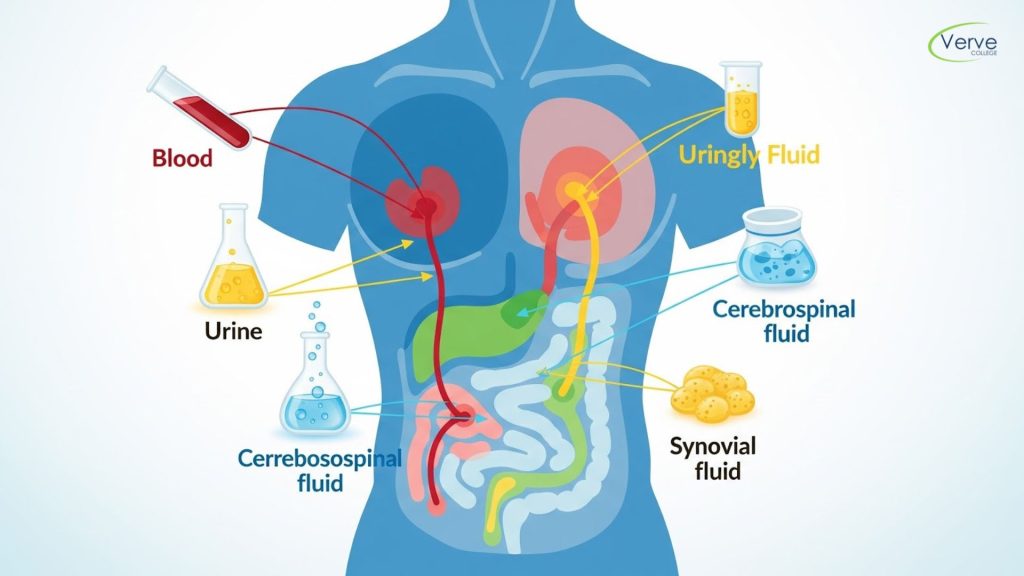
Types of Body Fluids: A Guide for Nursing Students
Types of Body Fluids: A Guide for Nursing Students
Studies in nursing education show that more than 60% of clinical decision-making depends on correctly understanding body fluids and their role in health and disease. From detecting infections to monitoring organ function, body fluids provide critical clues about what is happening inside the human body. For nursing students, learning this topic early builds a strong foundation for patient care, diagnostics, and clinical confidence.
Many students encounter this topic during anatomy and physiology classes near me, where body fluids are introduced as part of core human biology. This guide explains the types of body fluids in clear, simple language, helping nursing students connect theory with real-world clinical practice.
Key Takeaways
- Body fluids help maintain balance, transport nutrients, and remove waste
- Each type of fluid has a specific function and clinical importance
- Changes in fluid color, volume, or composition can signal disease
- Nurses regularly assess body fluids during patient monitoring
- Understanding fluids improves accuracy in clinical observations
Types of Body Fluids and Their Clinical Importance
Blood
Blood is the most vital body fluid and plays a central role in oxygen delivery, immune defense, and waste removal. It consists of plasma, red blood cells, white blood cells, and platelets. Plasma carries nutrients, hormones, and electrolytes, while red blood cells transport oxygen throughout the body.
From a nursing perspective, blood analysis helps detect anemia, infections, clotting disorders, and chronic illnesses. Monitoring blood loss, transfusions, and lab values is a daily responsibility in clinical settings. Understanding blood composition allows nurses to recognize early warning signs and respond quickly to patient needs.
Lymph
Lymph is a clear fluid that supports the immune system and helps remove excess fluid from tissues. It travels through lymphatic vessels and contains white blood cells that fight infection. When lymph flow is disrupted, swelling known as lymphedema can occur.
Nurses often observe lymph involvement in conditions such as infections, cancer, and post-surgical recovery. Swollen lymph nodes can indicate immune activity or disease progression. Learning about lymph in an A&P Class helps students understand how immunity and fluid balance work together in the body.
Cerebrospinal Fluid (CSF)
The brain and spinal cord are encased in cerebrospinal fluid, which serves as a cushion.It also supplies nutrients to the nervous system and removes metabolic waste. CSF is clear and colorless under normal conditions.
In nursing practice, CSF analysis is used to diagnose conditions like meningitis, multiple sclerosis, and brain hemorrhage. Any change in color, pressure, or composition is clinically significant. Nurses play a key role in patient preparation, monitoring, and post-procedure care during lumbar punctures.
Synovial Fluid
Synovial fluid is found in joint cavities and reduces friction during movement. It allows joints to move smoothly while absorbing shock. Healthy synovial fluid is clear and slippery.
Nurses may encounter synovial fluid assessment in patients with arthritis, joint infections, or injuries. Thickened or cloudy fluid can indicate inflammation or infection. Understanding this fluid helps nurses support mobility, pain management, and rehabilitation care.
Pleural Fluid
Pleural fluid exists between the lungs and chest wall, allowing smooth breathing by reducing friction. Normally, only a small amount is present.
Excess pleural fluid, known as pleural effusion, can cause breathing difficulty and chest discomfort. Nurses monitor respiratory status, assist with thoracentesis, and observe fluid drainage. Recognizing abnormal pleural fluid helps nurses act quickly in respiratory emergencies.
Urine
Urine is a waste fluid produced by the kidneys and reflects hydration status, kidney function, and metabolic health. Its color, clarity, and volume provide valuable diagnostic clues.
Nurses regularly assess urine output, especially in hospitalized and critically ill patients. Changes in urine can signal dehydration, infection, or kidney disease. Accurate monitoring supports early intervention and patient safety.
Saliva and Digestive Fluids
Saliva aids digestion and protects oral health, while gastric and intestinal fluids help break down food and absorb nutrients. These fluids are essential for maintaining nutritional balance.
Nurses observe digestive fluids when caring for patients with gastrointestinal disorders, feeding tubes, or dehydration. Abnormal secretions may indicate ulcers, infections, or digestive dysfunction.
Why Understanding Body Fluids Matters in Nursing?
Understanding body fluids strengthens clinical judgment and patient assessment skills. Nurses rely on fluid observations to detect early symptoms, prevent complications, and support recovery. This knowledge becomes especially important during clinical rotations and patient interactions.
Students who master these concepts in an A&P nursing class often feel more confident transitioning from classroom learning to real-world nursing care.
Conclusion
A clear understanding of the types of body fluids helps nursing students connect anatomy, physiology, and patient care into one complete picture. Each fluid plays a unique role in maintaining balance and signaling health conditions. By learning to recognize both normal and abnormal changes, nurses can provide safer and more effective care. This foundational knowledge supports clinical accuracy, improves patient outcomes, and builds long-term professional confidence.
Frequently Asked Questions (FAQs)
- Can body fluid changes appear before symptoms?
Yes. Changes in body fluids often occur before visible symptoms, making early detection possible. - Are body fluids tested differently in children and adults?
Yes. Normal ranges vary by age, so interpretation depends on the patient’s developmental stage. - Do medications affect body fluid composition?
Many medications can change fluid levels, color, or chemical balance, requiring close monitoring.
 Sign up
Sign up Login
Login




